ROBERT PIERCE
• Leader & Times
Medicaid continuous enrollment associated with the federal Public Health Emergency due to the COVID-19 pandemic ended in March 2023 in a process called “unwinding,” which requires re-review of participant eligibility.
Those no longer deemed eligible or those who fail to meet eligibility deadlines may lose access to the federally funded health coverage program.
“During the pandemic, the federal government incentivized states to keep people on Medicaid so they wouldn’t be at risk of losing their health coverage,” Kansas Health Institute Senior Analyst Sheena Schmidt said. “For a little more than three years, they did not have to complete a renewal process to get their Medicaid eligibility redetermined.”
With the end of the PHE came the end of the continuous provision eligibility, and Schmidt said states were then charged with resuming renewal eligibility processes. This has been taken place during the last year, and Schmidt said Medicaid clients were sent renewal letters to let them know to reapply.
Schmidt said a number of things have to be done to reapply for Medicaid, including confirmation of contact information, reporting of income and household situation. The Kansas Department of Health and Environment then reviews that information to determine based on income level and other factors if a person is eligible for Medicaid and to have coverage continued.
Schmidt said thus, states are unwinding from the PHE’s continuous coverage provision.
“KDHE, we understand, completed their unwinding in terms of sending out all the renewal letters and determining whether or not the individuals on Medicaid were eligible as of May 31, but they are still operating with some flexibilities CMS, the Centers for Medicare and Medicaid Services, have allowed through this process so as to not take people off of Medicaid or discontinue their coverage for a procedural reason or for any other reason other than they’re not eligible,” she said.
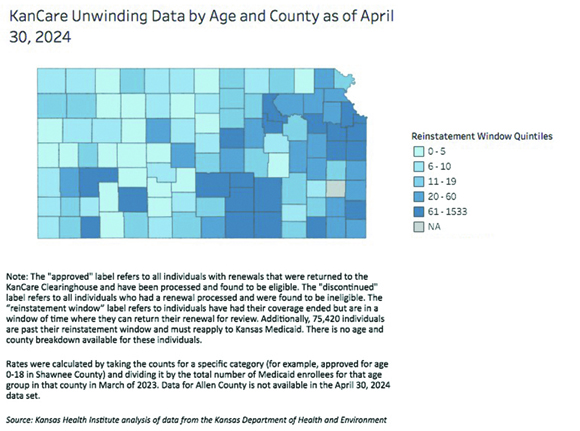
KHI analyzed KanCare renewal data as of April 30, the most recent available, and developed an interactive map to show Medicaid unwinding status by age, group and county. Schmidt said the map provides a detailed breakdown that helps Kansans understand the demographics and geographic distribution of those affected by the unwinding process.
“There’s been several categories by which they’re collecting data and tracking information,” she said. “It gives stakeholders an idea of how the process is going in each county and how it’s affecting children versus adults. There’s a variety of ways you can look at the data.”
CMS has extended unwinding through June 30, 2025. Schmidt said about half of those who still need to provide information to the state are in the reinstatement window or children.
“Initially, there were a lot who were losing coverage or having children,” she said. “Other organizations in the state tried to do outreach and encourage families to submit that information so their children can retain coverage either on Medicaid or CHIP (Children’s Health Insurance Program).”
As of April 30, there were 318,791 approved and 75,532 individuals who have their coverage discontinued. Another 15,078 members were in the reinstatement window and have 90 days to submit their renewal for review. Schmidt said bigger states have different unwinding strategies, and this makes comparing Kansas’ status to other states difficult.
“The enrollment during the pandemic was higher than it had ever been due to that continuous coverage,” she said. “We expect it to be lower after this process completes.”
Schmidt said KDHE primarily determines Medicaid eligibility, but the Kansas Department for Aging and Disability Services plays a part in the process too. She added certain things in the unwinding process have some flexibility as a way to minimize the number of people who are getting potentially limited coverage for a procedural reason.
“It maintains consistent eligibility standards, and they were trying keep contact information for people up to date so they didn’t disenroll anyone on the basis of returned mail and the state was making a good effort to contact individuals so they could get their updated information and determine eligibility,” she said. “They’re conducting all the reviews with federal requirements. They’re also implementing strategies about doing member messaging and outreach, partnering with stakeholders and managed care organizations to get information update for folks, automating as many processes as they can and allowing members to update their contact information online.”
Schmidt said KDHE is also facilitating transitions to other affordable coverage, including local health insurance navigator resources for individuals who lost coverage due to the renewal process.
“Whatever category you’re in, whether you’re a parent or whatever family circumstance you have, it’s based on income and household size and if you have a certain condition,” she said. “There are various other eligibility requirements based on the population group you would be classified under for Medicaid.”
For those who are on disability or pregnant or have certain health conditions covered by Medicaid, Schmidt said this is likewise taken into consideration with regards to the income level a person must reach in order to retain coverage.
“CHIP is part of Medicaid, and their income level and household size is a higher level than it would be for traditional Medicaid,” she said. “For children, the federal poverty limit is 255 percent of FPL. It’s lower for parents. For childless adults in Kansas, even if you’re income is zero, you do not qualify for any Medicaid no matter what.”
Schmidt said those who are 65 and older qualify for Medicare, but childless adults with disabilities and medical conditions may still qualify for Medicaid. At this point, she said she believes renewals have been sent out to all Medicaid clients in Kansas.
“They’ve completed that process, and they’ve either determined eligibility for those who have returned their renewal paperwork, and they’ve placed them in a reinstatement window, which means they’re in a 90-day window to return their paperwork,” she said.
Schmidt said if individuals are determined eligible, they may have their coverage backdated to when it was discontinued.
“There’s another group of people which has a sizeable amount in it where they need to submit a new application,” she said. “Their window has passed. They no longer have coverage, but if they submit a new application, they would be able to determine their eligibility at that time and potentially regain coverage if they’re eligible.”
A total of 75,420 members have been placed in the “new application required” category because their reinstatement window has passed.
Nearly all states were initially expected to complete “unwinding-related” renewals such as the first renewal conducted for each individual enrolled in Medicaid or CHIP at the end of the continuous enrollment condition by June 2024.
However, due to state adoption of strategies to prevent inappropriate disenrollments and other CMS-approved unwinding-related strategies, many states will continue conducting unwinding-related renewals beyond June 2024 for some populations.
“Other states definitely had issues,” Schmidt said. “CMS was thinking we need to set a pause. Kansas around June of last year paused their discontinuations to do some catchup and to adjust some of their processes because many people were getting discontinued for procedural reasons.”
Schmidt said inappropriate disenrollments occur for several reasons, including income information not being updated and a lack of paperwork or information at the time they are needed.
“People only initially have 30 days once they receive the renewal letter to return the information in the mail, which is not sufficient for even allowing people to submit their information in a timely manner,” she said. “If they didn’t receive it in time, they could’ve had their coverage discontinued even if they were still eligible.”
As officials with KDHE took pauses and took a look at readjusting the unwinding process, Schmidt said they were able to catch up on some of the work needed to be done to help with unwinding.
“They adjusted staffing,” she said. “They adjusted a few other things and reported back to the legislature on what they were doing in order to comply with the guidance on that.”